Documentation, Tracking and Real-Time Analytics
APCTrakker™
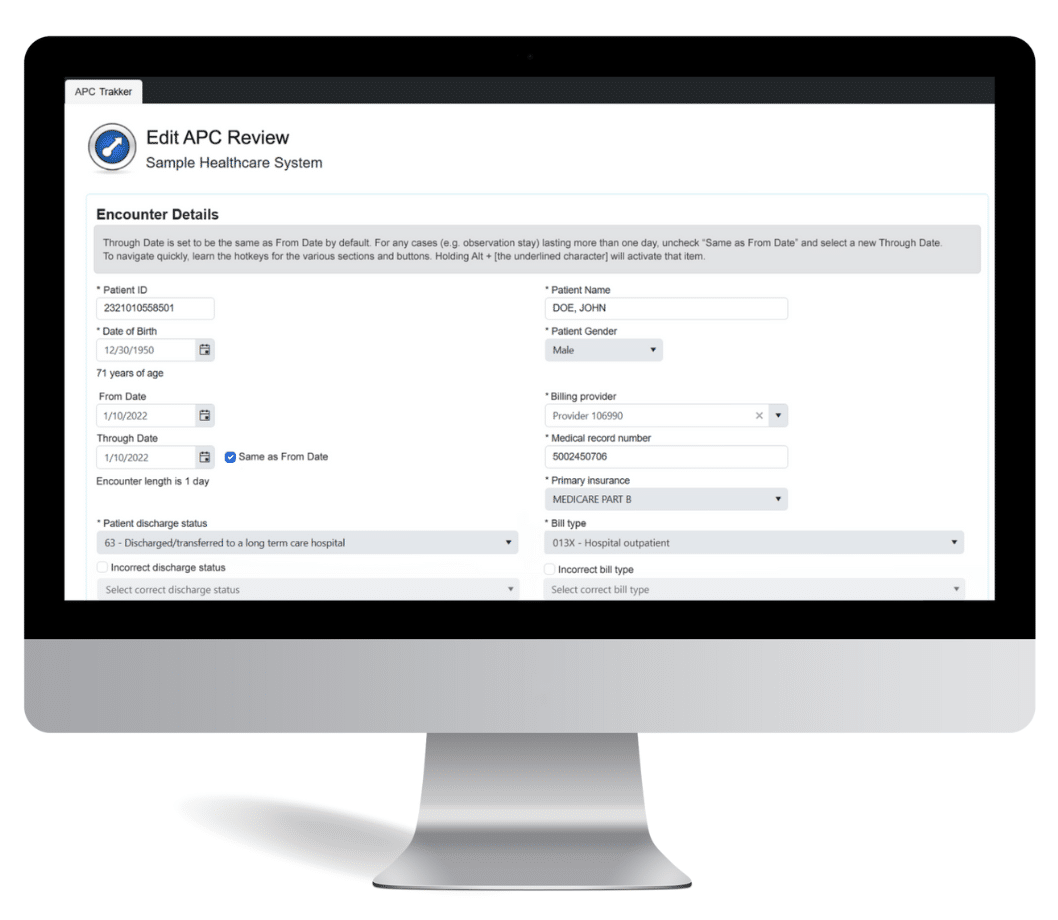
APC Trakker is the premier tool for auditing hospital outpatient reimbursement. Easily import your outpatient facility claims in bulk into this powerful online tool and audit all aspects of the claim. Using the CMS grouper, it instantly validates the accuracy of the billed APC code to ensure complete and accurate reimbursement.
APC Trakker captures APC-specific variables, including ICD-10 diagnosis codes, HCPCS procedure codes, and modifiers to determine whether the billed APC was supported. Auditors can flag any errors or issues for subsequent review and, where appropriate, deliver coder and provider education.
APCTrakker Features
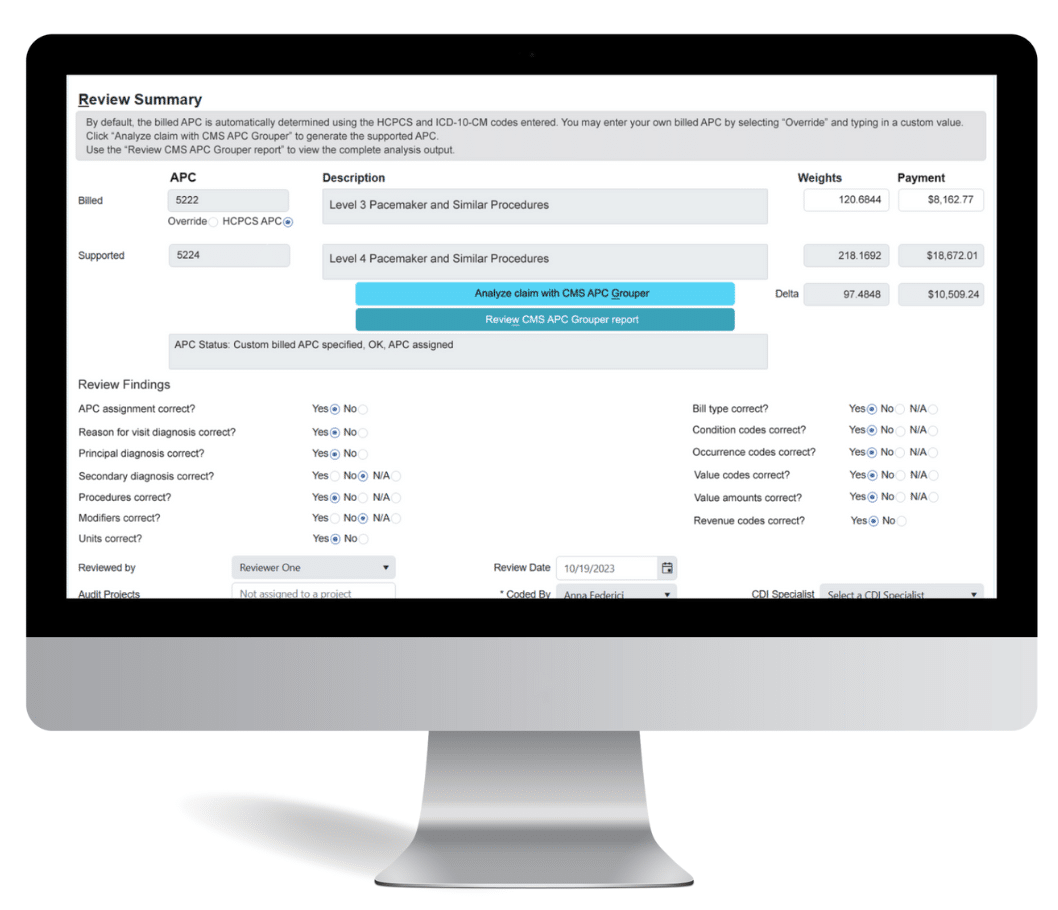
Audit Summary and I/OCE Report
APC (Ambulatory Payment Classification) Trakker generates detailed audit reports for you to review with coders and providers. After the claim information is populated, APC Trakker’s Audit Summary allows you to validate the billed APC to determine if it’s supported. The Summary displays the APC weights for the billed and supported APC, as well as the delta. You can also configure APC Trakker to show the corresponding reimbursement in unadjusted Medicare dollars, based on the claim year’s OPPS fee schedule. APC Trakker uses Medicare’s “Integrated” Outpatient Code Editor (I/OCE) to process your claim data exactly as Medicare would, and you can choose to display the actual I/OCE output as well.
Coding Accuracy and Error Checking
In addition to importing data, you may also manually populate the APC Trakker review form with claims data. APC Trakker comes with error checking capabilities that will catch obvious errors, such as reporting codes on CMS’ inpatient-only procedures list. If a hospital outpatient claim turns out to contain inpatient services, you can import the claim into DRG Trakker, our inpatient facility auditing module.
Ready to see how it works? Book a demo today.