Health Systems’ Secret to Managing Audit Risk
DRGTrakker™
Created with acute care inpatient hospitals in mind, DRGTrakker goes beyond benchmarking. Audit targets are assessed and prioritized — all without opening a single chart. This will give your internal audit team a straightforward head start on risk reduction.
DRGTrakker Features
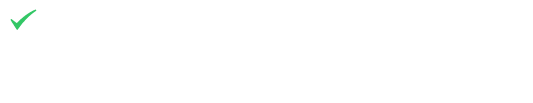
Precision Assessment
Preparing for an upcoming audit, or avoiding an audit in the first place, requires a health system to look at their coding habits through the payers’ eyes. To simplify this, DRGTrakker includes a comprehensive set of audit targets drawn directly from OIG, RAC, PEPPER, and many other up-to-date, official sources. Project organization and custom targets enable you to provide better-targeted education utilizing risk-based audits generated by the system. Your team will be able to monitor trend data to catch higher-priority risks or likelihoods of getting audited months earlier than a probe audit process.
The Review Process
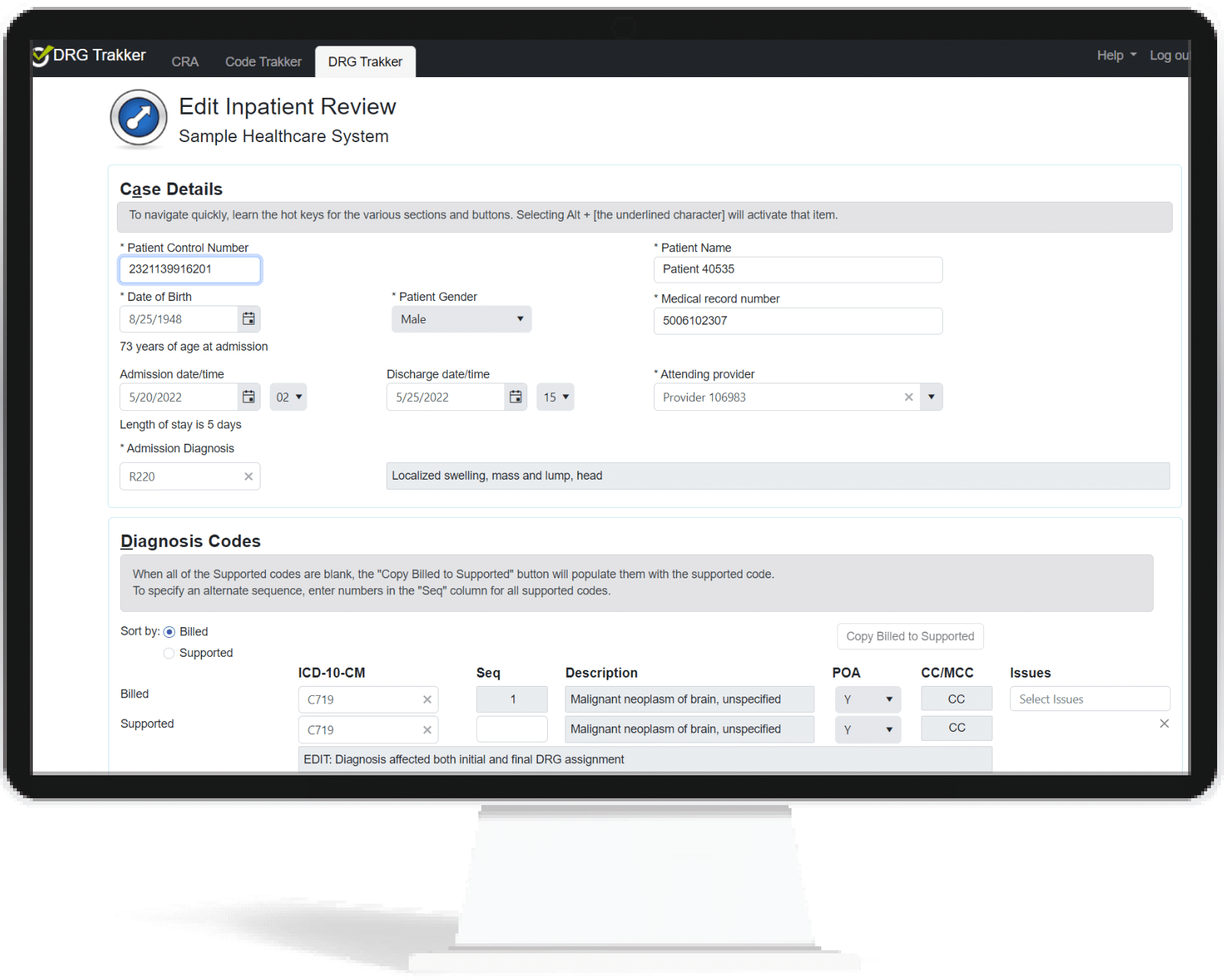
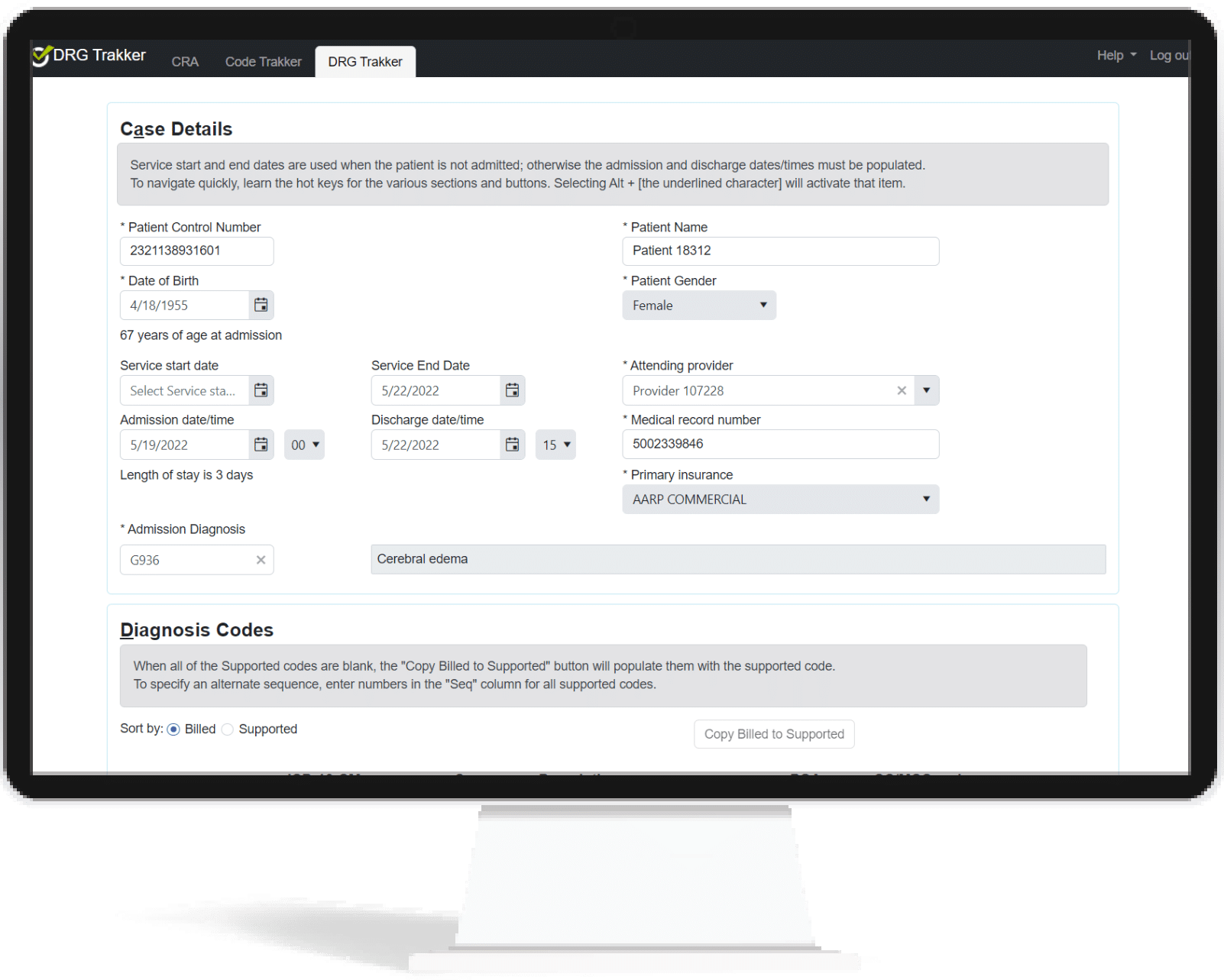
The review process is also streamlined. Based on the audit targets risk model, reviewers can easily define the universe of claims with which to work and select a sample to review. The generated reviews have the majority of the form pre-populated and placed in the reviewers’ queue. Entering the supported codes and findings is easy and with efficiency boosters such as:
- Indicate billed diagnosis and procedure codes are supported with one click – useful when there are a dozen codes that are correct (or mostly correct).
- A custom notes library – lets you save and insert custom notes to ensure standard and error-free messages are delivered to providers.
- MS DRG grouper is built-in to calculate the financial impact of any modifications.
A full set of analytical reports are available, including:
- Re-Bill Financial Impact
- Coder Accuracy
- Detailed review reports for education and remediation
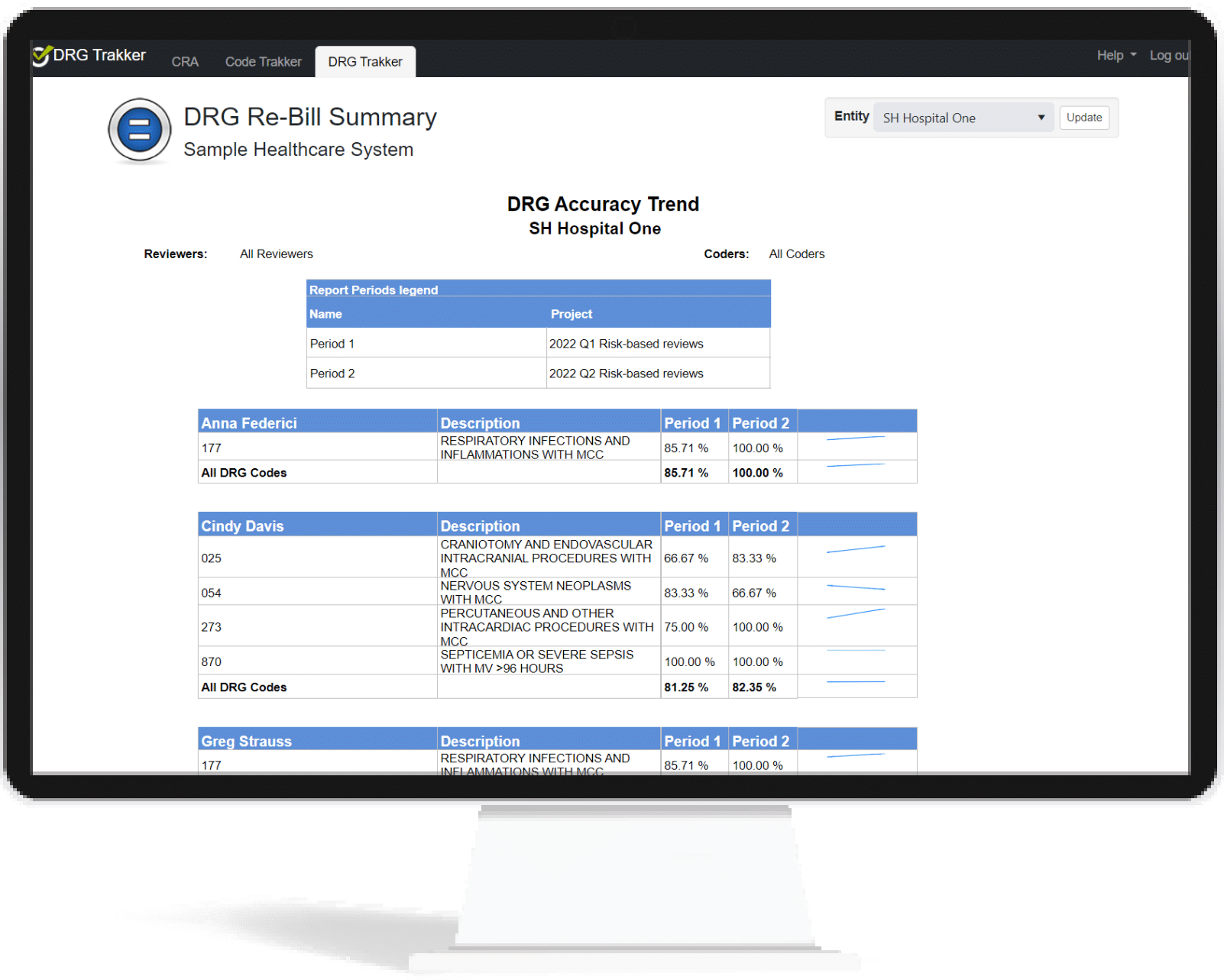
- Coding and DRG Accuracy trend data
Complete Coding Vigilance
One of the biggest challenges that audit managers face is determining which providers or codes are creating the most risk for your organization. CRA gives you an instant, top-down look at your organization’s current compliance health. DRGTrakker provides trend data over time to see which coders or coding components present ongoing risk, empowering your team to confidently employ education and remediation to reduce the possibility of an audit.
Education and Remediation
CRA supports fostering continued education within each audit project. DRGTrakker offers guidance as you’re working, outlining what claims need to be corrected on the project you’re currently in. It goes a step further by identifying where education is needed.
After initial education has been conducted, CRA will generate analytic and trend reports based on the outcomes of current coding practices. Continuous analytic reports summarize which risks persist and which have newly emerged. By providing a complete overview of your education and remediation results at a glance, teams are able to address risks quickly and produce a higher percentage of clean claims.