Real-Time Audit Documentation
CodeTrakker™
CodeTrakker is your tool to capture procedure and modifier reviews of physicians and APP providers. This is where the top coding issues facing your organization, identified by CRA, are put into a solutions-based action plan.
Claim samples are generated based on CRA’s risk assessment or any external events. Your team’s findings are used to provide feedback to the analysis engine, continuously improving the results for maximized efficiency over time.
CodeTrakker™ Features
The Review Process Promotes Auditor Productivity
Using the audit plans generated by CRA or your compliance policies, reviewers can easily define the universe of claims with which to work and select a sample to review. Reviews are generated with the majority of the form pre-populated and placed in the reviewers’ queue. Entering findings is straightforward and has efficiency boosters such as:
- An evaluation and management code scoring engine – fully document your findings and CodeTrakker will determine the correct level of service.
- A custom notes library – lets you save and insert custom notes to ensure standard and error-free messages are delivered to providers.
CodeTrakker Analytics
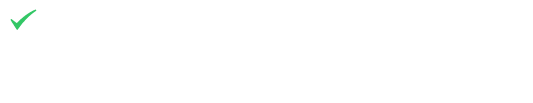
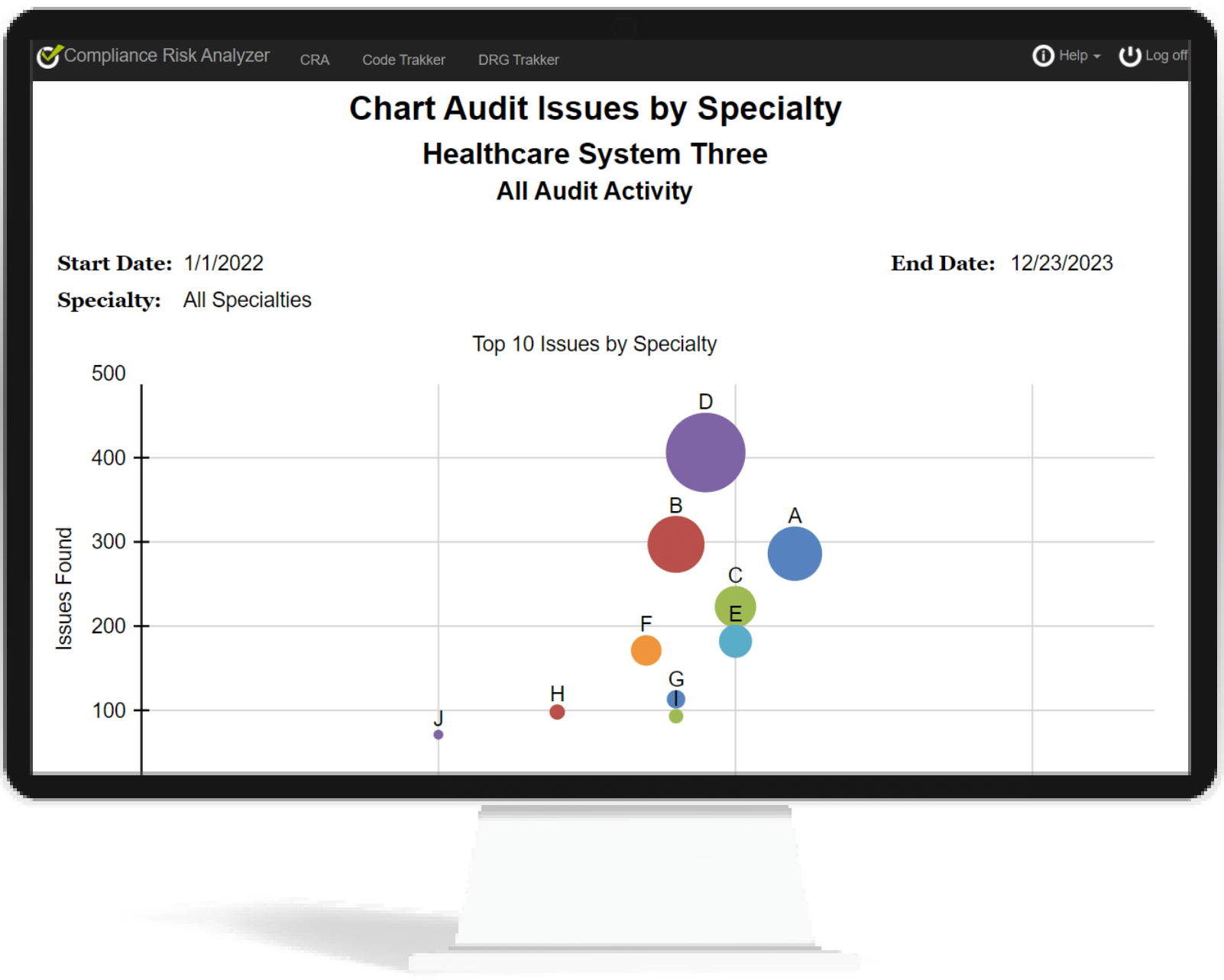
With CRA’s many tracking features, organizations are transformed into an agile, accurate coding compliance team, making significant improvements with speed and precision. Analyze and monitor:
- Education and Remediation Efficacy
- Coding Behavior
- Issues with a high likelihood of being audited
- Actions that are causing the increased risk
- Accurate coding habits that are currently in practice
- Coders who need improvement
- Trend of Coding Accuracy
- Reviewer Productivity
Reporting
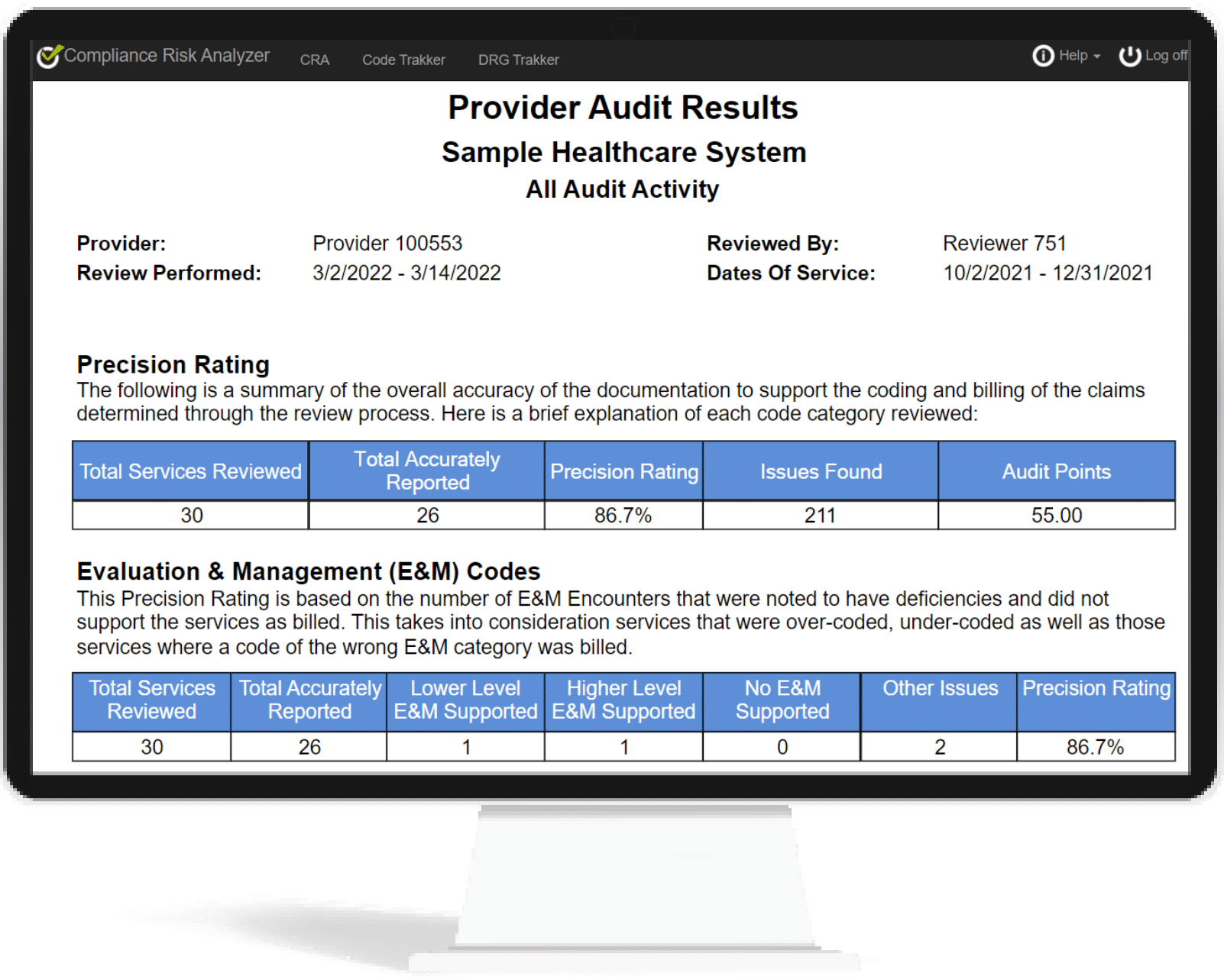
CodeTrakker generates a detailed audit report for you to review with your providers. The report identifies any codes that were not supported and clearly highlights the underlying components that led to selecting a different code. This simplifies the process of determining why the reviewer disagreed with the billed code and serves as a convenient education step.
You can customize the appearance and content of these reports, saving you time and giving you a valuable educational tool to streamline the provider education and feedback process. The report will give providers the ability to review the findings and cite exactly where and why a billed code wasn’t supported.